together,we’vegot this
WHAT WE DO
Dedicated support for your patients and your practice
PTC Cares™ is a personalized resource that works to help patients get started on treatment, continue treatment uninterrupted, and be supported throughout their treatment journey. We’re here to help with:
- Benefits investigation and prior authorization support >
- Financial assistance information and support >
- Specialty pharmacy coordination and refill reminders >
- Connecting families with community resources, including Peer Navigators >
- Continuous support—as a dedicated single point of contact, we’ll be here to help when you need us
Starting treatment and activating PTC Cares
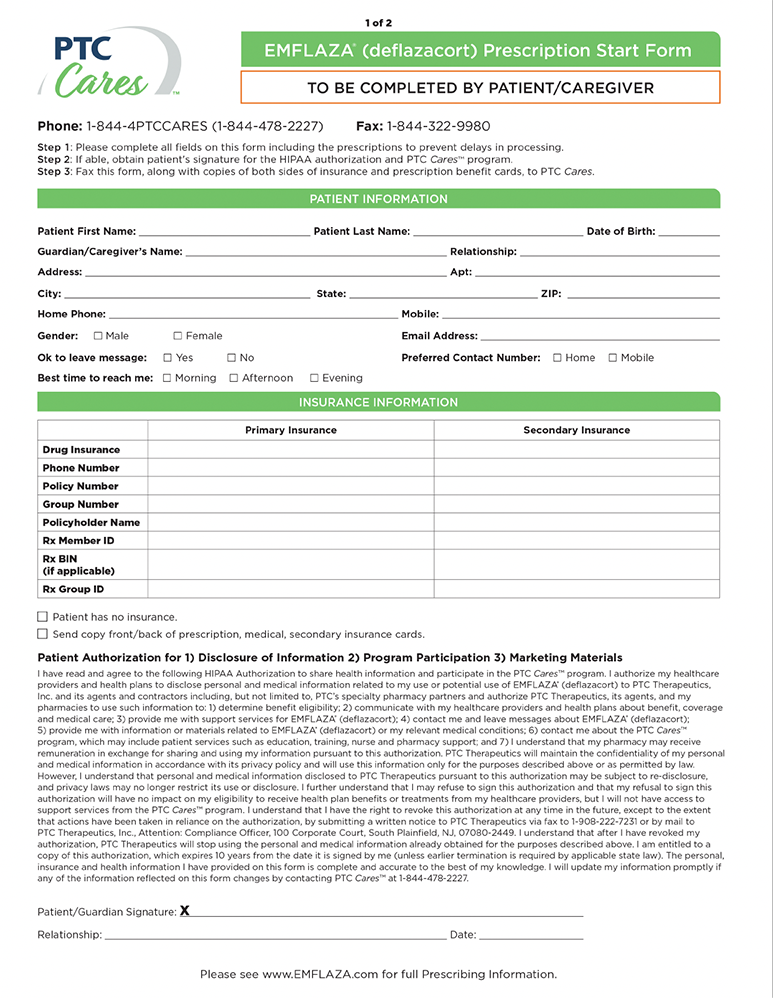
Prescription Start Form
The first step in beginning treatment is the Prescription Start Form. There are two pages: one for you and one for your patient or their caregiver. Once both pages are completed and signed, simply fax them to the number on the form (1-844-322-9980) to start the prescription process.
REMEMBER: It’s important to ensure that both pages are fully completed and that both the prescriber and the patient or caregiver sign the form before it is submitted.
case managers
Personal attention. Personalized support.
With PTC Cares, your Case Manager will serve as your primary communication hub, connecting your office, your patient, and the patient’s payer and specialty pharmacy throughout treatment. As a dedicated single point of contact, Case Managers can help make sure that your patients and your practice are well-informed and personally supported.

Courtney
PTC Cares Case Manager

Rick
PTC Cares Case Manager
FINANCIAL ASSISTANCE
Always working to support treatment access
Insurance benefits differ widely, and out-of-pocket costs are often variable. We’ll explore every possible option to help keep affordability issues from blocking your consented patients’ access to the treatment you prescribe. PTC Therapeutics offers several programs to help meet eligible families’ needs, depending on individual circumstances:
The Copay Assistance Program*†
can help qualified families who have commercial insurance cover out-of-pocket costs associated with treatment.
The Bridge Program*
can provide consented patients who are actively enrolled in PTC Cares a temporary supply of PTC medication free of charge while they are waiting for verification of insurance coverage.
If a family needs additional financial support, we’ll help them connect with other charitable patient foundations that may be able to help.
*Low to no out-of-pocket costs for most patients who qualify.
†Not valid for prescriptions eligible to be reimbursed, in whole or in part, by Medicaid or Medicare (including Medicare Part D), or where prohibited by law.
specialty pharmacy
Getting medication where it needs to be, when it needs to be there
For many families, working with a specialty pharmacy may be a new experience. We’ll be there to guide patients and their families through the specialty pharmacy process at every step, from the first prescription through every refill.
Specialty pharmacy initiation
We’ll work with the family, the payer, and the specialty pharmacy to manage all the details to help ensure access to treatment.
Help scheduling deliveries
We’ll help families coordinate deliveries to ensure that medication arrives on time, every time.
Provide refill reminders
We’ll proactively monitor when refills are due and provide reminders to schedule them.
Support beyond treatment
Connecting your patients with additional resources
Our commitment to helping families who live with Duchenne extends far beyond treatment. By working with our PTC Therapeutics Patient Engagement partners and other groups in the Duchenne community, PTC Cares Case Managers can help families connect with additional support.
Peer support
Our Peer Navigator Program connects patients and caregivers with other families who understand their journey and can share stories and advice.
Local resources
We’re connected with the Duchenne community at the local and regional level, so we can help direct your patients and their families to the resources that are most relevant to them.
Patient advocacy groups
We help families connect with patient advocacy groups that provide education, resources, and other support.


